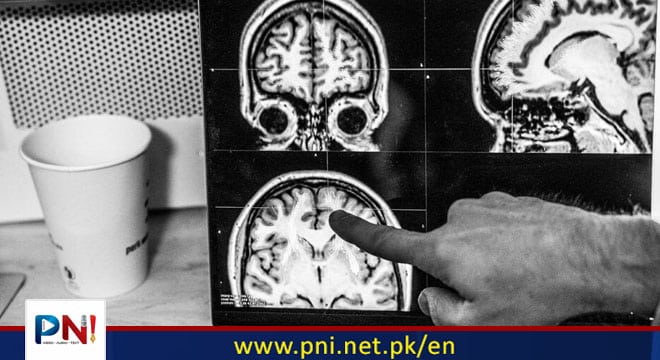
ISLAMABAD, May 13 (Online): An observational study examines how age-related changes to white matter in the brain could impact recovery following a stroke. Rosem Morton for The Washington Post via Getty Images
Recovery after a stroke can be unpredictable and influenced by many factors.
An observational study examines how age-related brain changes could be linked to stroke recovery.
The authors suggest a possible link between age-related damage to parts of the brain containing white matter and stroke recovery.
When a person has a stroke, the damage that has been done to the brain only partially predicts whether a person may recover their motor control.
An international group of scientists has discovered that areas of the brain known as white matter hyperintensities (WMH), thought to be related to age, could be used to predict outcomes after a stroke.
The observational study, recently published in Neurology, used MRI images to measure the area of the brain damaged by a stroke. The study specifically examined white matter hyperintensities, which are sites of damage in the brain.
The researchers found that age-related changes in the brain’s white matter influenced stroke recovery.
Lead study author Sook-Lei Liew, PhD, associate professor at the USC Keck School of Medicine Department of Neurology and the USC Viterbi School Department of Biomedical Engineering in Los Angeles, told Medical News Today:
“Our study is one of only a handful to demonstrate a relationship between WMH and motor control after stroke and is part of a bigger movement, from our lab and others, to examine the impact of global brain health on stroke motor recovery. We are continuing to investigate other global brain health markers on post-stroke motor recovery — we have been studying the impact of brain aging and are currently looking at the relationships between WMH and other brain health measures.”
Recovery from stroke linked to aging white matter
Using data from the ENIGMA Stroke Recovery Working Group, researchers tracked 223 stroke patients across seven research sites in four countries.
Participants were asked about their motor control symptoms, and those taking part in the study were at different stages of recovery after their stroke, with data collected an average of 147 days post-stroke.
Researchers discovered that white matter hyperintensity size and the area of the brain affected by stroke were both positively associated with motor control symptoms.
The researchers also found that for people with fewer white matter hyperintensities, their motor control symptoms were more associated with the size of the area affected by the stroke.
In contrast, for people with larger white matter hyperintensities, their symptoms exhibited a greater correlation with cortical spinal tract damage.
There were no significant differences observed between males and females.
The authors suggest their findings could show that white matter hyperintensities modify an individual’s recovery of motor control after a stroke.
What causes white matter hyperintensities?
White matter hyperintensities appear as they do on MRI scans since they represent areas where fluid is accumulated.
They are present in over half of people over 60 and are associated with aging.
These areas have been shown to increase with age and are correlated with cognitionTrusted Source and risk of Alzheimer’s disease (AD), though understanding of their cause is inconclusive.
“White matter hyperintensities are a radiological finding most commonly identified on a Fluid Attenuated Inversion Recovery (FLAIR) sequence of magnetic resonance imaging (MRI) brain scans,” José Morales, MD, a vascular neurologist and neurointerventional surgeon at Pacific Neuroscience Institute in Santa Monica, CA, not involved in the study, explained to MNT.
“White matter hyperintensities specifically refer to lesions found in the white matter tracts of the brain, i.e., the cables connecting neurons, and are an imaging biomarker for diseases affecting/damaging the cells, i.e., oligodendrocytes, that insulate these tracts,” he added.
Previous research has shown that white matter hyperintensity volume is correlated with shorter telomere length.
Telomeres are repetitive sequences of non-coding DNA that exist at the end of the chromosomes and shorten each time a cell divides, meaning that as we age, the telomeres in our cells shorten.
“WMH are white matter lesions in the brain that are thought to be due to reduced blood flow and/or ischemic damage (due to vascular disease),” Liew said.
“They can be due to a lot of things, but recent research finds that they also be reversed. They are commonly associated with cognitive decline and risk of stroke and other vascular disorders. It is thought that lifestyle modifications to reduce high blood pressure can be very beneficial.”
Inflammation and ischemic injury were two known mechanisms known to cause white matter disease and white matter hyperintensities, Morales explained.
“In the case of the latter, ischemic demyelination occurs due to small vessel disease. WMHs affect the conduction of electrical signals between neurons, which may impact also impact neuroplasticity and compensatory neural network activity. Both are mechanisms employed by the brain to recover from brain damage, such as stroke.”
— José Morales, MD, vascular neurologist and neurointerventional surgeon
More research on aging white matter and stroke recovery needed
The next steps for the researchers could be identifying biomarkers of white matter hyperintensities, Morales suggested.
“Novel imaging sequences and serum assays are being developed that may reliably identify upstream biomarkers of small vessel disease and abnormal blood-brain barrier opening, both of which putatively lead to the appearance of white matter hyperintensities. It is important to note that white matter hyperintensities are downstream epiphenomena of covert cerebrovascular disease,” he said.
“While primary prevention is the best prevention, early secondary prevention still has great potential to significantly and positively impact many people at risk for end-stage disease such as stroke or dementia,” Morales concluded.
What happens to the brain as we age?
There are various changes that happen to the brain as a person ages. These include changes in memory, the ability to multitask, the ability to learn something new, and more.
The effects of aging on the brain can vary from person to person.
Slowing down brain aging or stopping it altogether would be the ultimate elixir to achieve eternal youth. Is brain aging a slippery slope that we need to accept? Or are there steps that we can take to reduce the rate of decline?
At around 3 pounds in weight, the human brain is a staggering feat of engineering, with around 100 billion neuronsTrusted Source interconnected via trillions of synapses.
Throughout a lifetime, the brain changes more than any other part of the body. From the moment the brain begins to develop in the third week of gestation to old age, its complex structures and functions are changing, networks and pathways connecting and severing.
During the first few years of life, the brain forms more than 1 million new neural connections every second. The size of the brain increases fourfold in the preschool period, and by age 6, it reaches around 90%Trusted Source of its adult volume.
The frontal lobes are the area of the brain responsible for executive functions, such as planning, working memory, and impulse control. These are among the last areas of the brain to mature, and they may not develop fully until around 35 years of ageTrusted Source.
Follow the PNI Facebook page for the latest news and updates.